Ever wonder about pelvic organ prolapse and what it means? Well, here is everything you need to know!
Q: Where are my Pelvic Floor muscles?
A: The muscles create a hammock that go from your pubic bone (in front) to your coccyx (in back) as well as side to side. The pelvic floor muscles consist of three layers; the superficial layer can be found externally and internally while the two deeper layers can only be found internally.
Q: What is the job of the pelvic floor muscles?
A: These muscles support your organs, provide sphincteric control to help maintain bladder and bowel contents, and contribute to sexual function.
Q: Ok but what exactly do these muscles do?
A: In order to urinate, pass a bowel movement, or achieve orgasm the Pelvic Floor muscles need to relax and expand. In order to prevent urinary or fecal leakage the pelvic floor muscles need to be strong and remain active. For a variety of reasons the pelvic floor muscles can become weak, spastic, or restricted leading to difficulty with bowel movements, urination, or sexual function.
Q: What is Pelvic Floor Physical Therapy (PF PT)?
A: Physical therapists are musculoskeletal experts, this applies to the pelvic floor muscles as well. A physical therapist works with the client on re-training the Pelvic Floor muscles to work properly. An underactive Pelvic Floor (example: prolapse, weakness, urinary incontinence, postpartum issues) requires a strengthening/up-training program, whereas an overactive pelvic floor (example: constipation, chronic pelvic pain, sexual dysfunction) requires relaxation/down-training program.
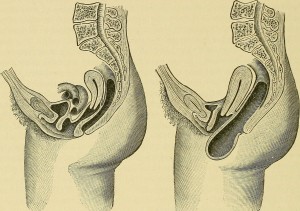
Q: How do my Pelvic Floor muscles relate to my prolapse?
A: The job of the pelvic floor muscles is to support your organs. If the pelvic floor muscles are weak they will be unable to support your organs. This lack of muscular support will cause the organs (often times the bladder or rectum) to descend which is known as a prolapse.
Q: How can Pelvic Floor Physical Therapy help my prolapse?
A: PF PT works on re-training and strengthening the muscles through an up-training program to better support your organs. Once the muscles that support your organs are strengthened the organs will have a better support system and not descend.
Q: Should I just do kegels all day every day and hope the prolapse resolves? If I don’t have a prolapse should I be doing kegels to prevent a prolapse?
A: Kegels are great WHEN they are done correctly. Unfortunately most people do not know how to properly engage their pelvic floor muscles and perform the kegels. People tend to substitute with their inner thigh muscles or gluteal muscles instead. This is why in certain countries, such as France, women are sent to PF PT after giving birth to learn how to properly perform kegels and strengthen their pelvic floor muscles. In order to prevent substitutions it is beneficial to see a PF PT to ensure proper pelvic floor muscle activation.
Q: If I haven’t yet seen a PF PT but was diagnosed with a prolapse is there anything I can do in the meantime?
A: Yes! There are certain positions that will alleviate the pressure placed on your organs providing you with some much needed relief. Gravity is working against you and your prolapse putting pressure on the organs, when you take the pressure off the organs you allow gravity to work in your favor. One of the positions is to lay on your back on the floor with your feet up on the couch alternatively you can lay on your back with your hips elevated upon pillows or a wedge. Finally downward dog is a yoga position that helps temporarily pull the organs back into alignment.