Can AI Help Catch Breast Cancer? The Surprising Answer.
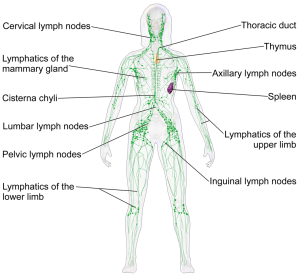
October is almost upon us! Every year, we see the famous pink ribbons that mean another Breast Cancer Awareness Month has arrived. Unfortunately, even with all the progress that’s been made, women are still being diagnosed with and dying of breast cancer in large numbers. The World Health Organization reported that as recently as 2020, over 2 million people received a breast cancer diagnosis and 685,000 succumbed to breast cancer. Those who survive breast cancer are lucky, but they are also more likely to face a range of health challenges even after they’ve been treated — including lymphedema and pelvic floor issues. For all women affected by breast cancer, we owe it to them to do everything to help them survive and thrive.
So, what is AI, anyway?
AI, or Artificial Intelligence, utilizes computers and machines to mimic human performance, and that includes the performance of doctors! AI can check you for skin cancer, discover if you have COVID-19 by hearing you cough, and interpret mammograms. Pretty amazing, right?
Why doctors need help from AI
Although we don’t like to think about it, a radiologist could possibly miss breast cancer while reading a mammography. Did you know, in fact, The National Cancer Institute believes that approximately 20 percent of breast cancers may remain undiagnosed after mammograms? And as we all know, early detection and treatment for breast cancer can make all the difference.
AI has the potential to help mammography become a more powerful breast cancer detection tool, allowing it to discover 20% more breast cancers, according to the initial results of a Swedish study published in August of this year. The doctors in the study also spent 44% less time looking at mammograms, thanks to AI. Less time with images equals more available time for patients, and any patient who has been rushed by a stressed doctor can see the potential benefits of that!
What AI means for the future of breast cancer screening
This doesn’t mean AI will or should put doctors out of business. Computer scientist Peter Kecskemethy, co-founder of Kheiron Medical Technologies, told The New York Times, “An AI-plus-doctor should replace [a] doctor alone, but an AI should not replace the doctor.” Humans are still vital to providing healthcare—that’s not changing any time soon! But powerful tools can make us more powerful healthcare providers. In the same way physical therapists rely on tools like foam rollers and dilators to supplement care, these radiologists may some day rely on AI.
AI may not be used at your next mammography, but it might eventually. I look forward to reading more about AI’s potential in all aspects of healthcare, as I have a feeling we haven’t even seen the tip of the iceberg.
https://www.politico.eu/article/ai-improves-breast-cancer-detection-rate-20-percent-swedish-study/
https://www.nytimes.com/2023/03/05/technology/artificial-intelligence-breast-cancer-detection.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8661054/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9255500/