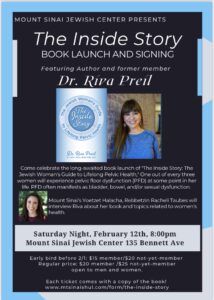
Come one, come all to the long awaited book launch party of The Inside Story: The Jewish Woman’s Guide to Lifelong Pelvic Health! On February 12, 2022, we will have the opportunity to celebrate my five+ years of work together at Mt. Sinai Jewish Center (MSJC). (Nope, not February 13, 2022 as originally planned because, who are we kidding, there is no competing with the Super Bowl. I wouldn’t miss one of my favorite annual events even for my own book launch!)
One out of every three women will experience pelvic floor dysfunction (PFD) at some point in her life. PFD often manifests as bladder, bowel, and or sexual dysfunction. How does one know if they are experiencing PFD during the various stages of their life, and what can be done to help address it? The Inside Story is a book designed to help ease life cycle transitions for Jewish women. It addresses the various pelvic health issues that may arise during the life cycle and provides practical exercises and guidance to help address it. The goal of the book is to share information about pelvic floor dysfunction and women’s health so that those suffering in silence can seek out appropriate treatment.
The program will include a conversation about the book and women’s health between me and Racheli Taubes, Rebbetzin and Yoetzet Halacha of MSJC. Event attendees will receive a copy of the book while enjoying fine wine and scrumptious cheese. Both women and men are invited and encouraged to attend.
The most exciting part about launching this book is that it gives me the opportunity to help an even larger audience. True, I am blessed to love my job tremendously, which includes one on one opportunities to educate my patients. However, too many women don’t even realize that physical therapy can be an invaluable modality to address their symptoms. I hope and pray that this book will help me educate MANY more women, and that it will be included in what I like to call the “Kallah Canon,” the list of books that Kallah teachers encourage their brides to read in preparation for marriage.
To quote Rabbi Yaakov And Rebbetzin Peshi Neuburger (Rav of Congregation Beth Abraham/Rosh Yeshiva at Yeshiva University and Rebbetzin of Congregation Beth Abraham/Educator at Manhattan High School for Girls), “In these pages Riva Preil opens a conversation, friendly and empathetic, instructive and informative, in which she highlights the tools of her craft which can give women confidence and comfort in many parshiyot of life. Her engaging balance of modesty and clarity will make this volume invaluable for kallah teachers who wish to replace fear and insecurity with joyful anticipation, as they prepare young brides for robust and fulfilling marriages.”
May God enable me to help as many women as possible on both the micro (day to day with my patients) and macro (The Inside Story) levels!
Link for event registration: https://www.mtsinaishul.com/form/the-inside-story