A recent poll about female bladder control confirmed a very saddening fact- too many women are suffering in silence. The University of Michigan Institute for Healthcare Policy and Innovation, in conjunction with AARP, conducted the national poll under the direction of Dr. Preeti Malani, a professor at the university with a specialization in geriatric medicine. Over 1,000 women between the ages of fifty and eighty responded to the survey. Some of the most disturbing statistics that emerged from the poll are as follows:
- Almost 50% of women in the targeted age bracket experience urinary incontinence
- Of these women, approximately 33% experience symptoms almost every day
- According to respondents, the most common triggers associated with leakage were coughing or sneezing (79%), while en route to the bathroom (64%), laughing (49%), and exercising (37%)
- Approximately 66% of these women have not discussed this with their physicians
- 41% of women experiencing urinary incontinence reported that this issue is either a “major problem” or “somewhat of a problem”
- Only 38% of poll respondents participate in a pelvic floor muscle strengthening exercise program
We live in society where marketing and misinformation has conditioned many to believe that urinary incontinence is simply par for the aging course. Adult diaper products and advertisements bombard us in our pharmacies and on television, and this subtly communicates the message that incontinence is inescapable. Too many women have been trained to believe that urinary incontinence is a normal part of the aging process. While continence may prove to be more challenging as one gets older due to physiological and hormonal changes, it is not inevitable.
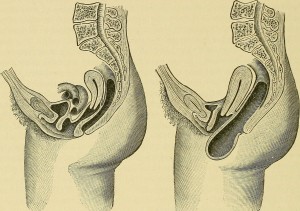
Pelvic floor muscle strengthening, or uptraining, is an evidenced based approach for improving continence. Women who experience urinary incontinence should discuss these symptoms with their doctors and request prescriptions for pelvic floor physical therapy. Obviously, this is a sensitive and delicate topic, and it is understandable that women may feel awkward initiating a conversation of this nature. However, it’s probably even more uncomfortable and depressing to resign oneself to a fate of eternal leaking.
If you or someone you know stands to benefit from a pelvic floor uptraining program, please contact us at Revitalize Physical Therapy. We specialize in treating men, women, and children experiencing urinary incontinence, and we can offer you a personalized treatment plan and home exercise program. We look forward to helping you along your healing journey!