While today’s blog title could have been stated by a number of my patients, it has been quoted, in fact, by none other than supermodel Chrissy Teigen. On April 20, 2016, she boldly tweeted about her post-partum urinary incontinence to her thousands of Twitter followers. Teigen isn’t the only one to publically discuss her postpartum problems on social media. In October 2015, Kim Kardashian West blogged on her website “Do you know you basically have to wear a diaper for two months afterwards?! LOL! No one told me that!” Stars truly are just like us, and even celebrities are susceptible to the musculoskeletal changes that occur during and after pregnancy.
The running theme that emerges from these celebrities, who are likely receiving top notch medical care and guidance, is “NO ONE TOLD ME.” Many women can probably relate to the frustration of incomplete patient education. After all, forewarned is forearmed, and it is understandable that women want to know what to expect when (and after) expecting! This blog is a response to the aforementioned complaint, and it will hopefully help women prepare in advance.
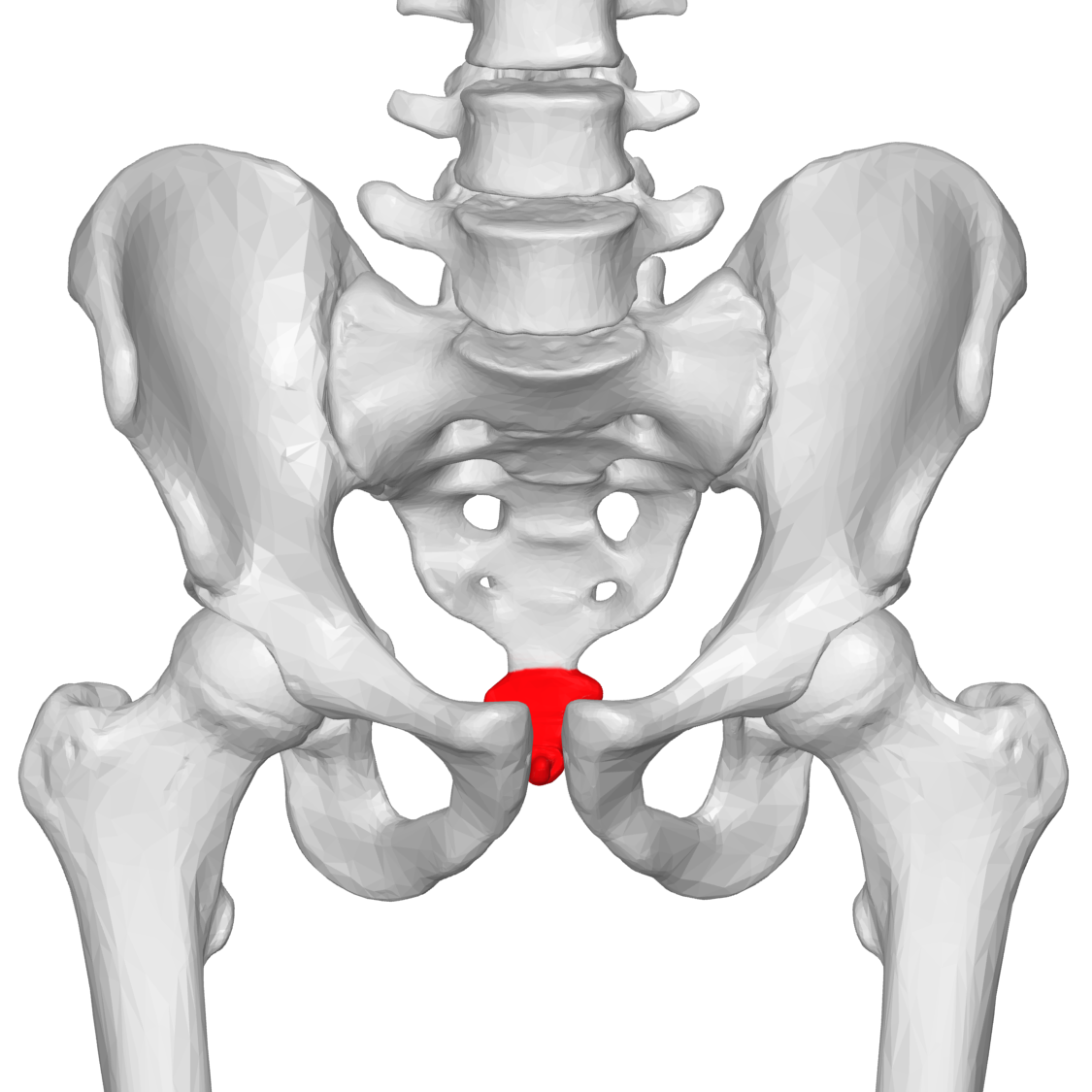
Both women who deliver vaginally and women who deliver via Caesarian section are subject to significant pelvic floor changes. The pelvic floor muscles, the muscles responsible for maintaining urinary and fecal continence, are subject to triple the amount of pressure compared to the non-pregnant state. Furthermore, increased amounts of the hormone relaxin, a hormone which loosens ligaments, circulate throughout the body to enable the pelvic expansion necessary for labor and delivery. When this occurs, the pelvic floor muscles can become overstretched and weak, thus impairing their ability to maintain continence.
While Kardashian West may believe that two months of diapers is par for the course for postpartum women, as a pelvic floor physical therapist I strongly disagree. Pelvic floor physical therapy is an excellent approach to address pregnancy related incontinence. Upon arrival to physical therapy, many women inform me that they have tried doing Kegel exercises but it has not made a difference. The truth of the matter is that approximately 50% of women who attempt to perform pelvic floor muscle exercises do so incorrectly. The most effective way to teach women how to utilize the proper muscles is via internal manual digital facilitation. One of my favorite moments as a clinician is sharing that “Aha!” moment with patients, i.e. when a patient experiences what it feels like to correctly contract their pelvic floor muscles for the first time (as opposed to the improper technique they had previously employed). Once a patient has properly identified the pelvic floor and how to engage it, biofeedback is another useful tool that physical therapists can use to train and strengthen the pelvic floor muscles.
Consider yourself educated, and please share this knowledge with other women. Let’s eliminate the “No one told me” component that frustrates so many new mothers and decrease the stress as much as possible. Not knowing what is happening within one’s own body adds to the other stressors experienced by postpartum women. Therefore, I encourage you to share this information with those who stand to benefit from it. Kudos to Teigen and Kardashian West for opening this conversation and normalizing previously tabooed topics.