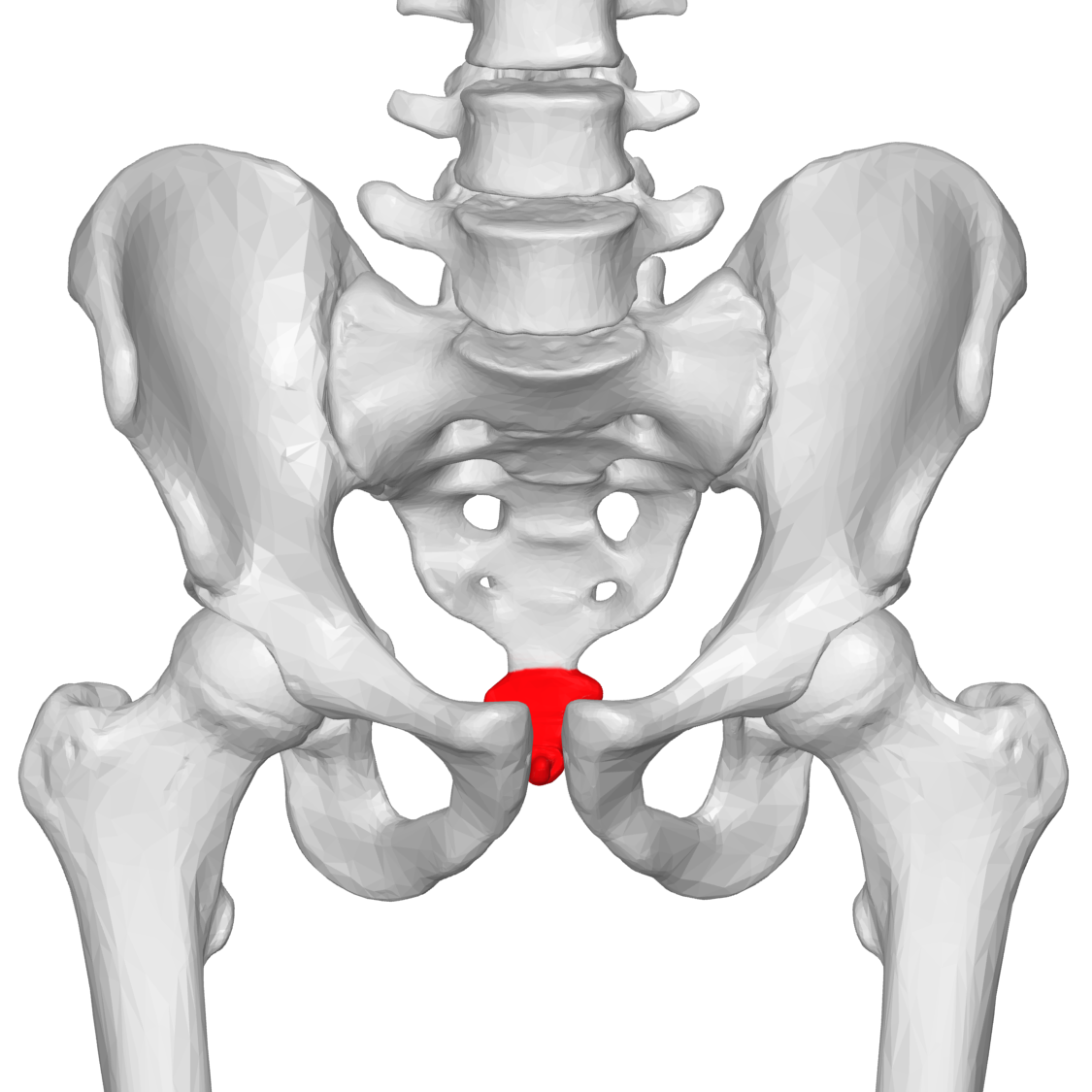
The coccyx, colloquially referred to as the tailbone, is a small, often overlooked anatomical landmark that sits below the lumbar spine and sacrum. Despite it’s tiny size, it is extremely clinically significant. Think of it as the Grand Central Station of your pelvic floor, so to speak. The coccyx serves as the attachment site of the gluteus maximus and levator ani muscles (which include the coccygeus, iliococcygeus, and pubococcygeus muscles) and ligaments (including the anterior, posterior, and lateral sacrococcygeal, sacrotuberous, and sacrospinous ligaments). Injury to the coccyx can affect the aforementioned muscles and/or ligaments. Conversely, injury to the muscles and/or ligaments can affect coccyx alignment. Symptoms of coccyx dysfunction include coccyx pain (referred to as coccydynia), pain with defecation, pain with intercourse, pain with prolonged sitting, pain with transitional movements (such as sit to stand), coccyx pain, low back pain, and even neck pain.
As per the title of this blog, the tailbone is often injured in one of two ways. It can either involve a traumatic onset, which involves a sudden and easily identifiable injury (ex. a sharp or painful fall), or an insidious onset, which is harder to pin point and often due to cumulative repetitive trauma. These traumas may include a history of chronic pelvic floor muscle tightness which can pull the coccyx out of alignment, or it may be related to a history of multiple minor falls or sports injuries (even during childhood) which seemingly “healed on their own over time.” As I often tell my patients, our musculoskeletal systems have a better memory than our brains, and what seemed at the time to be insignificant may in fact have a large impact down years later. My goal in stating this is NOT to produce fear or nervousness over waking up tomorrow with symptoms of tailbone pain due to unresolved previous injuries. Rather, my goal in sharing this information is to raise awareness and broaden your thinking; if you already DO experience any of the aforementioned symptoms, please consider that it may be due to the often overlooked coccyx.
Now that we have identified the importance of the coccyx and how it can become injured, let’s move onto the fun part…the part where physical therapists enter the scene…treatment and fixing the pain. The most common direction of coccyx injury is a “flexed” coccyx, or the coccyx becoming stuck in an anterior/forward position. Treatment of the coccyx involves external and internal mobilization of the coccyx to move it back into the proper position. Internal work can be accomplished through vaginal or rectal approach, depending on the patient’s comfort level and preferences. If the coccyx is deviated to either the right or left (in addition to or instead of a flexed coccyx), appropriate directional mobilizations are also indicated. In addition, the therapist may choose to tape the coccyx into the newly corrected position after treatment to help maintain the correction. Furthermore, as mentioned previously, the coccyx is attached to other structures, and therefore should not be treated in isolation. Any muscle or ligament tightness needs to be addressed in order to maintain the improved alignment. The final component of treatment is patient education about proper sitting posture, appropriate rest breaks to avoid prolonged sitting, and possible use of a donut or a different cushion initially for decreased pain.
If you or someone you know may benefit from pelvic floor physical therapy to treat an injured coccyx, please contact Revitalize Physical Therapy. I would love to have the opportunity to help you along your healing journey!